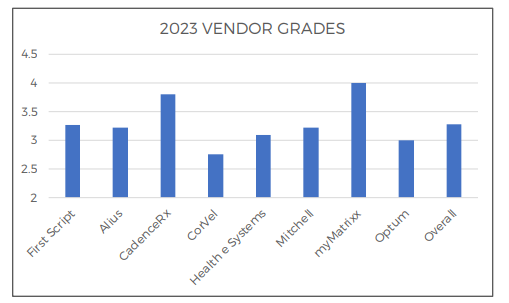
The industry has spoken and MyMatrixx by Evernorth continues its streak of being ranked the #1 pharmacy benefit manager (PBM).
For the 4th straight year in a row, MyMatrixx has earned the title of best workers’ compensation PBM in CompPharma’s Annual Survey Report.
CompPharma, an independent consulting and research firm, works with payers and pharmacy benefit managers (PBMs) to bring transparency into workers’ compensation pharmacy programs. Their most recent report surveyed 31 workers’ compensation professionals including decision makers, clinical personnel, and operations staff in state funds, carriers, self-insured employers, guarantee funds, and third-party administrators on the top PBMS and topics such as drug spend, pharmacy programs, and industry trends.
Combining their input with analysis of pharmacy data from 2022 and 2023, CompPharma released their 19th Annual Prescription Drug Management in Workers’ Compensation survey report on September 12, 2024.
We’re proud to set the standard in delivering the best client and customer service in the industry, earning us the title of top PBM in an increasingly competitive market. But while our PBM services and tools are number one, injured workers still come first—our focus remains on their recovery, safety, and successful return to work..