Our parent organization Evernorth has released its Health Care in Focus 2022 Report that reveals key insights in the healthcare industry for driving change and action. Evernorth partnered with Ipsos - a multinational market research and consulting firm – to conduct a U.S. survey of more than 3,000 consumers with employer-sponsored health insurance, as well as 575 human resources decision-makers (HRDMs) and 58 health plan leaders (HPLs).
The analysis of the data revealed:
- Success relies on a balanced, hybrid model that integrates in-person care with virtual solutions
- Despite greater interest and investment in behavioral health, plan sponsors and members could be better aligned
- Plan sponsors can benefit from partnering with members on affordability and access to care, in order to restore order amid the challenges of COVID-19
Broad Enthusiasm for Virtual Care/Telehealth
According to Evernorth’s recent report, virtual care has grown in both presence and popularity, with overall satisfaction among consumers remaining high. Consumers say they are very or somewhat satisfied with their virtual care experience across a variety of formats, including apps, text messages, video calls and traditional (audio) phone calls.
Virtual care, or telehealth, is a major topic widely discussed in the workers' comp industry as we continue to navigate the pandemic and find innovative solutions to provide effective care for injured workers. Key findings found that consumers are much more willing to embrace telehealth types of care and medical disciplines over others.
- A growing number of consumers are seeking virtual mental health counseling or therapy (up from 11% to 17% in 2021)
- Consumers are decidedly less enthusiastic about applying virtual solutions to other types of care such as physical therapy, which is the least conducive to virtual care
Universal Emphasis on Meeting Behavioral Health Needs
Did you know that therapy now represents the second-most common discipline for telehealth visits? Since the onset of COVID-19, consumers have embraced virtual care for mental health services. Behavioral health remains top of mind and a top concern in the medical community and general public.
From our own Phil Walls, myMatrixx Chief Clinical Officer, a large number of injured workers have been and continue to face mental health challenges in a pronounced and prolonged way compared to the rest of the population. Behavioral health problems, including depression and anxiety and social factors (such as isolation), can have a negative impact on long-term patient outcomes.
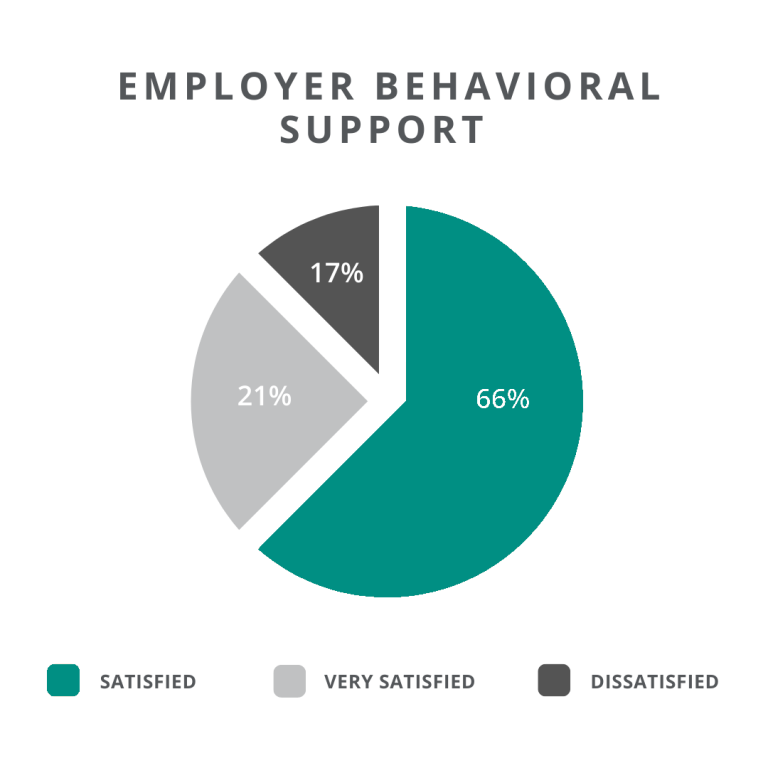
In workers’ comp and overall healthcare field, behavioral care plays a critical role in overall wellness and recovery for patients. According to Evernorth’s report, 66% of consumers report satisfaction with behavioral health support and benefits they receive from their employer and only a smaller subset of that satisfied segment expresses outright enthusiasm. This lukewarm response indicates an opportunity for plan sponsors to promote benefit offerings and to target their investments in the future.